This rare condition causes stabbing facial pain, even from a breeze – could you be at risk?
Specialists explain why the condition occurs, how it’s diagnosed, and the range of medical and surgical options available locally.

(Photo: iStock/Pornpak Khunatorn)

This audio is generated by an AI tool.
Imagine a sudden, electric shock-like pain striking one side of your face that can last seconds, at best, to a few minutes. The pain is so intense that it has been referred to as “suicide disease” by patients.
And it occurs several times a day when you’re chewing, talking, washing your face, brushing your teeth, or even having a light breeze blow across your face, according to Singapore General Hospital’s senior consultant Dr Adeline Leong, who heads its Department of Pain Medicine.
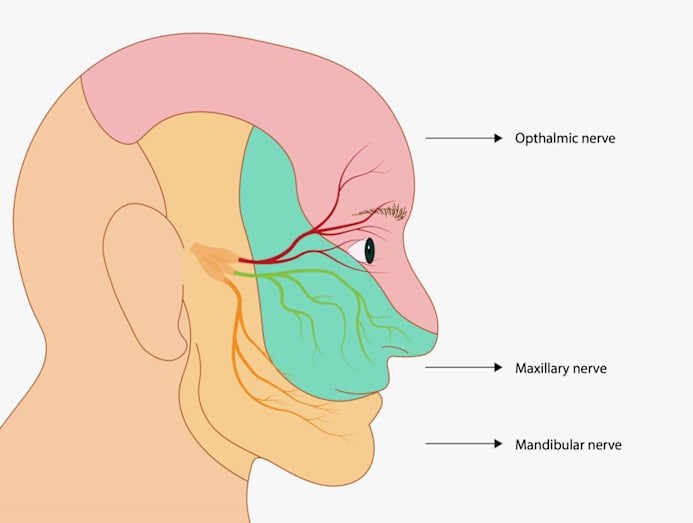
It's called trigeminal neuralgia (TN), a condition that affects the trigeminal nerve. There are two such nerves in your face, one on each side of your head. Each nerve starts in your brainstem (the part known as the pons) and travels across your face, where it splits into three branches to the eye as well as upper and lower jaws (see illustration below).
The trigeminal nerves’ locations explain why TN affects, most commonly, “the region below the eye involving the cheek bone and the jaw”, said neurologist Dr Tu Tian Ming from Mount Elizabeth Hospital. In addition to a stabbing pain, “some patients also describe a continuous dull pain in between episodes, which may fluctuate in intensity”, he said.
“Some patients report tingling or dull ache before severe pain begins,” added Dr Leong. “But often, the onset feels abrupt. The pain-free intervals can last weeks or months initially but can shorten over time.”
Here’s a look at what causes TN, how common is it, and the solutions available.
HOW COMMON IS TRIGEMINAL NEURALGIA?
TN is a rare condition. “There is no systematic collation of the number of TN patients in Singapore”, according to Dr Tu.
Associate consultant Dr Tan Chin Lik from National University Hospital’s Division of Neurosurgery, Department of Surgery, said that “the worldwide incidence is about four in 100,000”, which “translates into approximately 200 cases each year in Singapore”.
At SGH’s Pain Management Centre, “we see approximately 50 to 80 cases a year as a ballpark figure. Personally, I see about one or two patients in each clinical session,” said Dr Leong.
These patients are also seen in complementary care. Chiropractor and founder of Vitality Chiropractic, Shaan Daniel Rai, shared that “over the past seven years in operation, we have seen around 40 to 50 patients with TN. However, the incidence has been increasing over recent years, with three coming to see us in the past month”.

WHAT CAN CAUSE THE DEBILITATING PAIN?
The most common cause of TN – about 80 to 90 per cent of cases – is the compression of the trigeminal nerve by a loop of artery or vein, said Dr Tan. “Other causes include multiple sclerosis causing plaques in the brainstem, or a tumour compressing on the trigeminal nerve,” he said.
Situations that can affect the trigeminal nerve include head trauma such as whiplash, infections by the herpes zoster virus (it also leads to shingles), autoimmune conditions, circulatory issues, strokes, or accidental damage from brain, facial or dental surgery, according to Cleveland Clinic.
In addition, a study published in Neurology found that patients with high blood pressure were about 50 per cent more likely to develop TN than those with normal blood pressure over three years of follow-up. The researchers postulated that a twisted blood vessel, created by a high blood pressure, could compress the trigeminal nerve in these cases.
Migraine sufferers may be another group that can be prone to TN, according to Association of Migraine Disorders. Both migraine and TN affect the trigeminal nerve but in different ways: In migraine, triggers such as stress, light and hormones activate the trigeminal nerve's pain-sensing fibres; in TN, the same nerve is compressed. What links the two conditions is the “electrical activity in the brain is thought to activate the trigeminal nerve in migraine with aura”, noted the website.
Having said that, there are also many TN cases where there is no obvious cause, said Dr Tu.

WHO CAN BE PRONE TO TN?
“Patients are usually middle aged, from 50 to 70 years old,” said Dr Tan – although they can be younger, starting from age 20 to 30, said Dr Tu.
Women are more predisposed to developing TN than men. This could be due to women’s smaller nerve volumes, genetic predispositions and hormonal influences. In studies, women are also more likely to experience pain on the right side of their faces, while men are commonly affected on the left.
The reasons aren’t clear, although experts highlighted anatomical differences such as narrower bone openings on the right side of the female skull that could increase nerve compression.
“Most cases of TN are sporadic, that is, they are non-hereditary,” said Dr Tan, “although it is believed that a small percentage (1 to 2 per cent) may be so. Scientists have identified several genetic variants of ion channels (they control nerve functions), which may contribute to TN, but these require further investigations.”
WHAT ABOUT TREATMENTS?
A brain MRI is often ordered to look for a blood vessel compression, said Dr Tan. “MRI can also be used to identify tumour or demyelination plaques as a cause of facial pain.” Patients are usually managed by neurologists or pain specialists, and referred to neurosurgeons when surgery is being considered, said Dr Tan.
The common treatments available in Singapore include:
ANTICONVULSANT MEDICATIONS
These include carbamazepine and gabapentin, and they are often preferred as the first line of treatment as they are non-invasive, said Dr Leong. The downside, however, are the medicines’ side effects, including drowsiness, dizziness and nausea.
Downsides: “Some patients possess the gene, HLA1502, which increases the risk of a life-threatening rash known as Steven-Johnson syndrome when put on these medicines,” said Dr Tu.
“Carbamazepine, in particular, needs genetic screening beforehand,” said Dr Leong. “Carbamazepine also requires regular blood tests during the course of treatment to detect idiosyncratic reactions.”
Another downer, said Dr Tan, is that carbamazepine’s effectiveness may drop over time.
NERVE-BLOCKING INJECTIONS
Botox and steroids are often used for quick pain relief, and they can be done as outpatient procedures, said Dr Leong.
Downsides: The effects are temporary, lasting weeks to months. “There are also small risks of facial numbness, bruising or rarely, facial weakness,” said Dr Tan. “Sometimes, patients require repeat injections.”
GAMMA KNIFE RADIOSURGERY
After locating the trigeminal nerve through MRI, a frame is placed over your head and secured for precise positioning. A machine then delivers highly focused gamma rays on the trigeminal nerve to create a lesion and block the pain signals. Mild sedation is given before the procedure.

Since radiosurgery isn’t open surgery, it suits older or high-risk patients, or those whose neurovascular conflict is not found, said Dr Leong.
Downsides: A small risk of facial numbness or altered sensation. “There is also a latency period (weeks to months) before symptoms improve,” said Dr Tan.
RHIZOTOMY
A small needle or cannula is inserted through the cheek, near the corner of the mouth, and guided by X-ray to a small opening at the skull's base where the trigeminal nerve is located. From there, radiofrequency, sterile glycerol or balloon compression may be used to deactivate the pain fibres. Local anaesthetic is used for this procedure.
Rhizotomy is minimally invasive and offers quick relief, according to Dr Leong.
Downsides: The effects are temporary, lasting at least six months, said Dr Leong. Patients may also run the risk of facial numbness (sometimes, permanent) and anaesthesia dolorosa (severe burning pain in the numbed area), according to Dr Tan. “There is a higher recurrence rate compared to surgery.”

MICROVASCULAR DECOMPRESSION (MVD)
It involves accessing the trigeminal nerve through an incision behind the ear. After removing a small piece of the skull, the neurosurgeon finds the compressed nerve and moves the blood vessel away using biologic glue, a sling, clip or sponge.
“This surgical procedure is the most durable relief in cases where neurovascular conflict is found as it addresses the root cause,” said Dr Leong.
Added Dr Tan: “If done successfully, MVD allows preservation of the trigeminal nerve – anatomically and functionally – compared to rhizotomy. It also carries the highest success rate with lowest recurrence rate”.
MVD can have potential downsides, including hearing loss, stroke, infection or a longer recovery period, said Dr Leong.
HOW CHIROPRACTIC MAY HELP
“When there is a misalignment in the upper spine or neck, it can mechanically disrupt the nerves in the upper spinal cord and brainstem, including the trigeminal nerve,” said chiropractor and founder of Vitality Chiropractic, Shaan Daniel Rai. “This can be why patients experience associated neck pain or headaches, which can also come from this area.”
Before each session, patients have nerve scans taken “to help us assess progress and if we should or should not be giving the patient a corrective technique on that day”, said Rai. If needed, “this is all done with gentle, precise corrections; no big twisting, popping or ‘cracking’ of the spine”. The intention is to improve the alignment in the upper neck to reduce the mechanical tension placed on the nerves there and restore their functions. “With normal function, the nerve irritation reduces and pain improves,” he said.
Rai highlighted that “we work with neurologists, whenever possible, to suggest conservative approaches when the cause of TN is less clear”. “In these cases, if the doctor and patient agree, we would suggest upper cervical chiropractic care before resorting to surgery.”
“We encourage all patients to see a medical doctor for assessment, usually a neurologist, before seeking our care. This is to exclude any red flags that might warrant emergency surgery, such as a growth. However, most patients have already seen a plethora of doctors and practitioners before consulting us.”
He emphasised that “this isn’t to say surgery isn’t effective, but side effects can be possible”. “In my experience, it can be a longer and harder process for changes to occur due to the changes in the nerve after certain surgeries.”






